
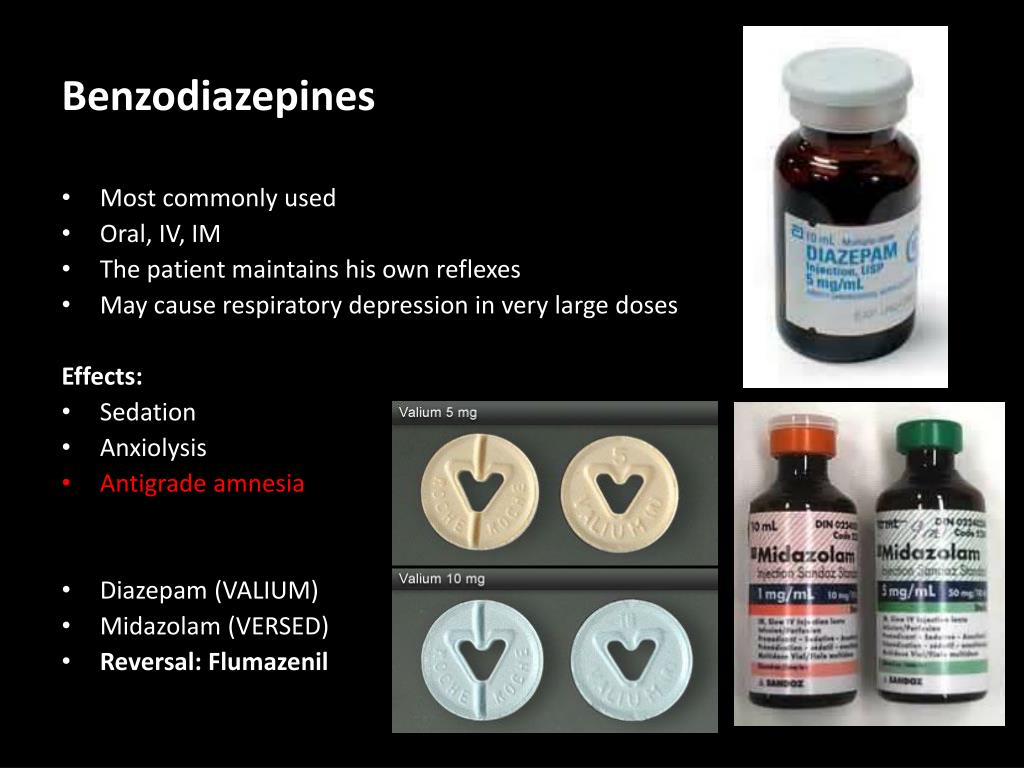
Oxygen-induced seizures are self-limited and do not increase susceptibility to epilepsy. The lowest possible concentration of oxygen that alleviates tissue hypoxia is optimal in patients with ARDS and decompensated neonates who are at particular risk for retrolental fibroplasia. Oxygen toxicity is managed by reducing the exposure to increased oxygen levels. Some chemicals such as the chemotherapeutic agent bleomycin also increase the risk of oxygen toxicity. Preterm newborns are at distinct risk for bronchopulmonary dysplasia and retrolental fibroplasia with prolonged exposure to high concentrations of oxygen. The incidence of displaying pulmonary symptoms with oxygen toxicity is 5%. This can occur after prolonged exposure to oxygen >0.5 ATA. The phenomenon of pulmonary toxicity is commonly referred to as the Smith effect. The incidence of displaying CNS symptoms secondary to oxygen toxicity is 2% with a seizure rate of 0.6%. However, this risk may be as high as 1 in 200 at higher pressures (2.8 to 3.0 times normal atmospheric pressure or one atmosphere absolute (ATA)) and as low as 1 in 10,000 for treatment at 2 ATA (atmosphere absolute air) or less. The overall risk may be as frequent as 1 in 2000 to 3000 treatments. This can occur with hyperbaric oxygen therapy in a dose-dependent corelation. The CNS effects secondary to oxygen toxicity is known as the Bert effect. This activity reviews the etiology, presentation, evaluation, and management of oxygen toxicity and reviews the role of the interprofessional team in evaluating, diagnosing, and managing the condition. Those at particular risk for oxygen toxicity include hyperbaric oxygen therapy patients, patients exposed to prolonged high levels of oxygen, premature infants, and underwater divers. Severe cases of oxygen toxicity can lead to cell damage and death. The acute toxicity manifests generally with central nervous system (CNS) effects, while chronic toxicity has mainly pulmonary effects. These two cases can result in acute and chronic oxygen toxicity, respectively. The clinical settings in which oxygen toxicity occurs is predominantly divided into two groups one in which the patient is exposed to very high concentrations of oxygen for a short duration, and the second where the patient is exposed to lower concentrations of oxygen but for a longer duration. However, breathing oxygen at higher than normal partial pressure leads to hyperoxia and can cause oxygen toxicity or oxygen poisoning. Get the latest news and weather delivered straight to your inbox.Oxygen is vital to sustaining life. $90,000 and 100% of project funding is subgranted through the Nebraska Department of Health and Services, Division of Behavioral Health.ĭownload our apps today for all of our latest coverage. The Narcan Program is funded in whole from SOR II #1H79TI083322 from Substance Abuse and Mental Health Services Administration Center for Substance Abuse Treatment. Mental confusion, slurred speech, or intoxicated behavior.Signs of opioid overmedication, which may progress to overdose, include: The person cannot be awakened from sleep or cannot speak.The person is vomiting or making gurgling noises.Fingernails or lips have a blue or purple cast.The face is extremely pale and/or clammy to the touch.Signs of opioid overdose, which is a life-threatening emergency, include the following: It can also occur when opioids are taken with other medications-for example, prescribed medications such as benzodiazepines (which include Xanax, Valium, Klonopin, and Versed) or other psychotropic medications that are used in the treatment of mental disorders-or with illicit drugs or alcohol.
For example, overdose can occur when a patient deliberately misuses a prescription, uses an illicit opioid (such as heroin), or uses an opioid contaminated with other even more potent opioids (such as fentanyl). Opioid overdose can be due to many factors.

Naloxone is not a controlled substance and cannot be abused, and only works if opioids are present in the system. Naloxone binds to the opioid receptors in the brain, preventing opioids from binding there, which can temporarily reverse an overdose. Common opioids include prescription medications used to treat pain, such as morphine, codeine, methadone, oxycodone, hydrocodone, fentanyl, and hydromorphone, and illicit drugs as heroin. Opioids are medications that act on receptors in the spinal cord and brain to reduce pain intensity and activate reward regions in the brain, causing the euphoria that can lead to misuse and opioid use disorder. Naloxone is an antidote to an opioid overdose.


 0 kommentar(er)
0 kommentar(er)
